Azoospermia is a condition where a man's semen contains no sperm, making natural conception impossible. It affects about 1% of all men and 10-15% of infertile men. Diagnosing Azoospermia Treatment is the first crucial step toward finding the right treatment and potential fertility solutions.
1. When Should You Get Tested for Azoospermia?
Men should consider testing for azoospermia if they experience:
Infertility Issues – If a couple has been trying to conceive for over a year without success.
Abnormal Semen Analysis Results – If previous tests indicate low or no sperm count.
Hormonal Imbalances – Symptoms like low libido, fatigue, or reduced facial and body hair may indicate issues with sperm production.
Past Medical Conditions – History of testicular injuries, infections, surgeries, or chemotherapy can affect sperm production.
2. How Is Azoospermia Diagnosed?
1. Medical History and Physical Examination
The first step in diagnosing azoospermia is a detailed medical history and physical exam conducted by a urologist or infertility specialist. The doctor will ask about:
Past medical conditions like infections, injuries, or surgeries affecting the reproductive organs.
Family history of genetic disorders that may contribute to infertility.
Lifestyle factors, including smoking, alcohol consumption, and exposure to harmful chemicals.
Sexual and reproductive history, including previous pregnancies or known fertility issues.
During the physical examination, the doctor checks for:
Testicular size and shape – Small or abnormal testicles may indicate sperm production issues.
Varicocele presence – Swollen veins in the scrotum can affect sperm production.
Hormonal imbalance signs – Enlarged breasts or lack of body hair may suggest low testosterone levels.
2. Semen Analysis
A semen analysis is the primary test to confirm azoospermia. The patient provides a semen sample, which is examined under a microscope to check for the presence of sperm.
If no sperm are detected in the initial test, a second semen analysis is recommended to confirm azoospermia.
If dead or immobile sperm are found, it may indicate severe sperm production issues rather than complete absence.
3. Hormone Testing
Hormonal imbalances can cause azoospermia. Blood tests measure levels of:
Follicle-Stimulating Hormone (FSH) – High levels indicate testicular failure (sperm production problems).
Testosterone – Low levels can suggest hormonal issues affecting sperm production.
Luteinizing Hormone (LH) – Helps regulate testosterone production in the testes.
Prolactin – High levels can indicate pituitary gland dysfunction affecting sperm production.
These tests help determine whether azoospermia is due to obstructive (blockage-related) or non-obstructive (sperm production issues) causes.
4. Genetic Testing
Some cases of azoospermia are due to genetic abnormalities. Doctors may recommend:
Y Chromosome Microdeletion Test – Checks for missing parts of the Y chromosome linked to sperm production.
Karyotyping – Identifies chromosomal disorders like Klinefelter syndrome, which can cause infertility.
Cystic Fibrosis Gene Test – Men with congenital bilateral absence of the vas deferens (CBAVD) may have cystic fibrosis gene mutations, leading to obstructive azoospermia.
5. Scrotal and Transrectal Ultrasound
Scrotal Ultrasound – Helps detect blockages, varicoceles, or structural abnormalities in the testes.
Transrectal Ultrasound (TRUS) – Checks for obstructions in the ejaculatory ducts or seminal vesicles that may be preventing sperm from reaching the semen.
6. Testicular Biopsy
If hormonal and genetic tests do not provide clear answers, a testicular biopsy may be performed. This involves:
Taking a small tissue sample from the testicles.
Examining it under a microscope for sperm production.
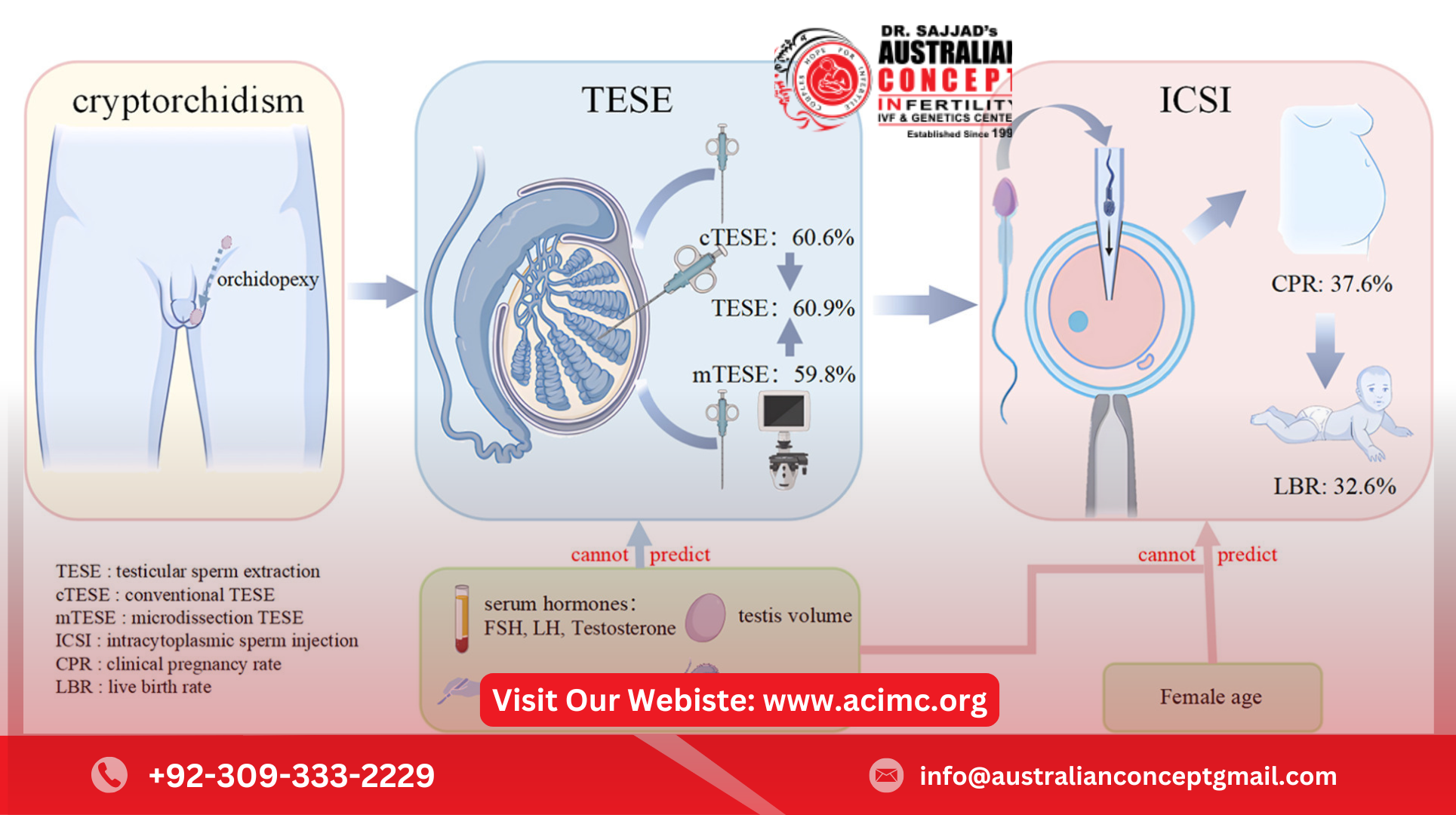
If sperm are found, sperm retrieval techniques like TESE (Testicular Sperm Extraction) can be used for assisted reproduction.
7. Post-Ejaculatory Urinalysis
If semen volume is low, doctors may perform a post-ejaculatory urine test to check for retrograde ejaculation (where sperm flows into the bladder instead of out through the urethra).
3. What Do the Diagnosis Results Mean?
After these tests, the doctor determines whether azoospermia is:
Obstructive Azoospermia (OA) – Sperm are produced but blocked from being ejaculated. This may be treatable through surgery or sperm retrieval for IVF/ICSI.
Non-Obstructive Azoospermia (NOA) – The testicles do not produce enough or any sperm, often due to hormonal imbalances, genetic conditions, or testicular failure.
4. Next Steps After Diagnosis
If azoospermia is due to an obstruction, surgical options like vasectomy reversal or sperm retrieval can be considered.
If it's due to hormonal imbalances, medication or hormone therapy may help improve sperm production.
If testicular failure is the cause, advanced reproductive techniques like IVF with ICSI using retrieved sperm may be the best option.
Conclusion:
Diagnosing azoospermia involves a step-by-step approach, including semen analysis, hormone testing, genetic screening, ultrasounds, and testicular biopsy. Early diagnosis helps determine whether treatment options like surgery, hormone therapy, or assisted reproductive techniques can improve the chances of conception.
For More Details: https://acimc.org/